Scientists at Stanford School of Medicine have made significant strides in diabetes research by successfully reversing type 1 diabetes in mice. This study, which used a novel approach that includes resetting the immune system and creating new insulin-producing cells, marks a promising step toward potential human applications.
The research, published in the Journal of Clinical Investigation, involved a multi-faceted strategy that combined a conditioning treatment with stem cell transplantation. Initially, a group of 19 pre-diabetic mice underwent a non-toxic conditioning regimen, which included low-dose radiation and specialized antibodies aimed at reducing the activity of T-cells, a type of immune cell.
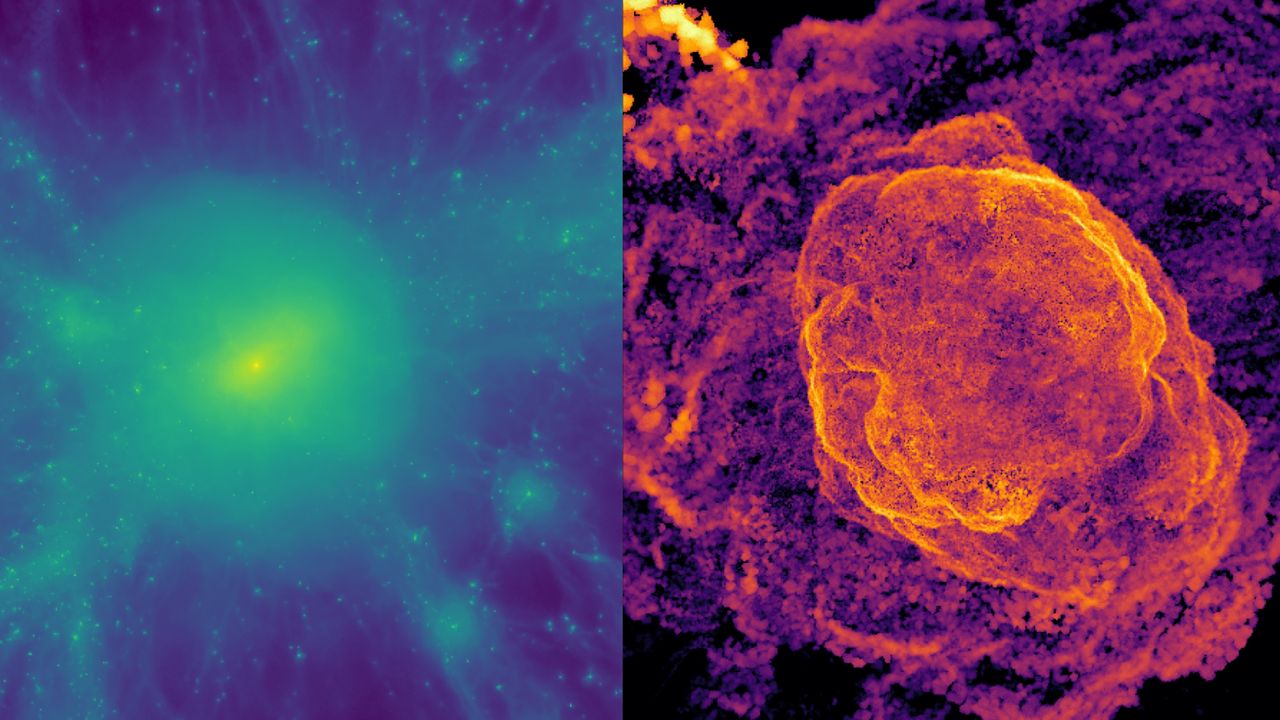
This conditioning phase aimed to make the mice’s immune systems less reactive, thereby creating a conducive environment for subsequent therapies. After this treatment, the mice received stem cell transplants using bone marrow cells from other mice, along with donor islet cells responsible for insulin production. This technique sought to establish a state known as “mixed chimerism,” where the recipient mice would possess a blend of their own cells and those from the donor.
The results were striking, as the approach effectively prevented diabetes in all 19 pre-diabetic mice. Following this success, researchers further tested their method on nine mice with established type 1 diabetes. Remarkably, all nine were completely cured after receiving the combined stem cell and islet transplantation protocol.
The absence of major side effects or significant immune depletion during these experiments is particularly noteworthy, as safety is paramount in assessing the efficacy of new treatments. While the study remains confined to animal models and involved some radiation, the research team expressed optimism about the potential for translating these findings to human medicine.
Potential Applications Beyond Diabetes
The implications of this research extend beyond type 1 diabetes. The conditioning approach could also serve as a viable treatment for various autoimmune diseases, such as rheumatoid arthritis and lupus, as well as non-cancerous blood disorders like sickle cell anemia. Dr. Seung K. Kim, a co-author of the study and a professor at Stanford University, described the methodology as potentially “transformative” for individuals not only with type 1 diabetes but also those requiring solid organ transplants.
Commentary from Dr. Marc Siegel, a senior medical analyst at Fox News, highlighted the preliminary nature of the findings but acknowledged their significant promise for future human treatments. He emphasized the need for modifications based on genetic analysis and artificial intelligence to tailor the treatment to individual patients. This personalized approach is critical, as autoimmune conditions like type 1 diabetes are complex and varied, suggesting that customized interventions may lead to more effective therapies.
The successful application of this treatment across different disease stages raises hopes for a paradigm shift in treating various illnesses. The ability to reverse and prevent type 1 diabetes in mice represents a crucial advancement in understanding the disease and opens the door to potential cures for humans in the future.
As research continues, the integration of a hybrid immune system—combining donor and recipient cells—could revolutionize treatment protocols, expanding the scope of stem cell therapies and offering new hope to patients battling autoimmune diseases. The findings from this study serve as a beacon of progress in the quest to understand and combat type 1 diabetes and other related conditions.