Research published in the journal Cell suggests that medications commonly prescribed for attention deficit hyperactivity disorder (ADHD) may not enhance attention as previously thought. Instead, these drugs, including Ritalin and Adderall, appear to target the brain’s reward and wakefulness centers, potentially increasing motivation and arousal levels in patients.
According to data from the Centers for Disease Control and Prevention (CDC), approximately one in ten children—about 11.4 percent—has been diagnosed with ADHD. Many of these children receive stimulant medications to help manage symptoms such as inattentiveness and impulsivity. The prevailing assumption has been that these stimulants improve attention networks in the brain. However, new findings challenge this notion.
Study Insights on Brain Functionality
Researchers at the Washington University School of Medicine conducted an extensive analysis involving MRI scans of 5,795 children aged 8 to 11 as part of the Adolescent Brain Cognitive Development (ABCD) Study. The analysis included 337 children who had taken stimulants on the morning of the scan and 76 who had prescriptions but had not taken their medication that day. The remaining participants had neither been prescribed nor taken any stimulants prior to the scan.
The researchers observed minimal differences in brain regions associated with attention—such as the dorsal attention network and the prefrontal cortex—between those who took stimulants and those who did not. In contrast, significant variations were noted in areas of the brain linked to reward and wakefulness. This suggests that the primary mechanism by which these medications operate may be through enhancing drive and motivation rather than focusing attention.
As Benjamin Kay, an assistant professor of neurology at the university, noted, “We’ve shown that the improvement we observe in attention is a secondary effect of a child being more alert and finding a task more rewarding.”
Connections to Sleep and Academic Performance
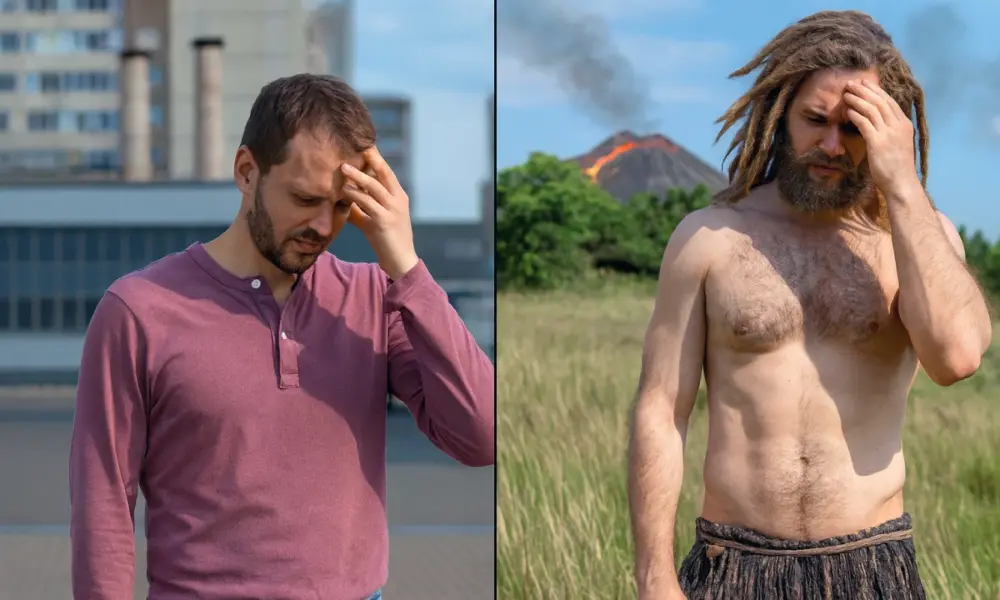
Further investigation revealed parallels between the effects of ADHD medications and sufficient sleep. The ABCD Study also provided insights into sleep patterns, grades, and cognitive test results. Notably, children with ADHD who received less than the recommended 9 hours of sleep per night benefited from stimulant use, performing better academically compared to similarly sleep-deprived peers who did not take the medication. Conversely, the stimulants had no significant impact on neurotypical children who were receiving adequate sleep.
Kay emphasized the importance of considering a child’s sleep patterns when diagnosing ADHD. “Not getting enough sleep is always bad for you, and it’s especially bad for kids,” he stated. He cautioned that while stimulants can alleviate symptoms like inattentiveness, they do not replace the necessity of good sleep.
The findings from this research not only contribute to the understanding of ADHD treatment but also call for a re-evaluation of how clinicians approach diagnoses and treatment plans. Parents, educators, and healthcare providers may need to consider the role of sleep in managing ADHD symptoms, reinforcing that medication should not be viewed as a substitute for healthy sleep practices.
This article is intended for informational purposes and does not provide medical advice. As research continues to evolve, it may lead to more nuanced approaches in treating ADHD and understanding the underlying mechanisms of stimulant medications.